In this post we will explore the ins and outs of large autoclave sterilizers, designated by the classification of EN 285 by the European sterilization standards and ANSI/AAMI ST79 by the American standards. Large autoclaves are found primarily in sterile processing departments, ambulatory surgery centers, laboratories and other medical clinics that require a large autoclave chamber for high-volume autoclaving.
How Does a Large Autoclave Work?
Let’s take a look at what happens inside one of these remarkable sterilizer machines. (The process is actually quite similar to the Class B tabletop autoclave, which we covered in our previous post.)
Just like with a conventional oven, we first need to preheat the autoclave, so it’s nice and hot when we are ready to sterilize the first load of the day. Once the autoclave is preheated via the autoclave jacket, we are ready to sterilize… (More on autoclave jackets later in this post.)
- We insert the load to be sterilized, set the autoclave to the appropriate cycle, close the door, and initiate the cycle.
- The first phase is removing the air from the autoclave chamber by vacuum pump in a series of negative pulses. If we were to use three pulses of 20 kPa to extract the air, they would work like this:
- The first pulse would extract about 80% of the air, leaving 20%.
- Then in the second pulse, 80% of the 20% remaining would be extracted (leaving 4% of the initial air).
- And finally the last pulse would remove 80% of the last 4% of air, which ultimately leaves 0.8% of the original air in the chamber.
- Now we begin the heat-up phase with positive pulses for distributing the heat and ensuring that every type of material, especially in a mixed load of plastics, stainless steel, aluminum, and glass, which have extremely different heat emissions, will reach the sterilization temperature. Positive pulses (as opposed to negative pulses, which remove air) pressurize the chamber by steam. The number of pulses are determined by the type and size of the load.
- The actual sterilization process begins now, also known as holding time. The pressure and temperature remain constant during this phase.
- At the end of holding time, sterilization is complete. Next the exhaust valve releases the pressure back to atmospheric pressure.
- We have reached the drying stage. The vacuum pump sucks out the moisture on the load by decreasing the pressure to lower than atmospheric pressure. In this way we create a vacuum inside the chamber and lower the boiling temperature to less than the actual boiling temperature of 100℃ (at sea level). This lower boiling temperature causes the water to evaporate into a gas, which is extracted by the vacuum pump, and behold, the load is dried!
- We have now reached the last stage, in which we equalize the pressure inside the chamber with the atmospheric pressure outside. Filtered air enters the chamber by way of a HEPA filter (at 0.2μm), which breaks the vacuum, so to speak, and returns the chamber pressure to ambient pressure.
- The sterilization cycle is now complete, and it’s safe to remove the load from the chamber.
Keeping the Chamber Hot with Autoclave Jackets
What is a jacket? The jacket is a stainless steel wall that surrounds the entire autoclave chamber. The space between the jacket wall and the chamber is filled with circulating steam to maintain the level of heat of the chamber walls.
In large autoclaves, we use jackets to preheat the stainless steel walls of the chamber in order to reduce the heating time and reduce the amount of steam that must be injected into the chamber. In addition, the jacket improves the drying stage by irradiating heat to the chamber in order to assist in the evaporation of moisture. This limits condensation during the prevacuum/heating phase; the more condensation there is, the wetter the load will get and the more difficult drying is.
In addition, the jacket isolates the chamber from colder ambient temperatures and prevents cold spots in the walls of the chamber, thus maintaining uniform heat distribution.
To get a visual demonstration of the jacket, check out our video about large autoclaves here.
Maximizing Large Autoclave Capacity with Space Constraints
Large autoclaves can range in size from 120 to 1300 liters. The question of which size to buy is generally complicated by the layout of the room in which the autoclave(s) will operate. Often hospitals, clinics, and laboratories need autoclaving solutions that maximize sterilization capacity in tight spaces.
In many European countries, steam sterilizers are designed to maximize STU capacity as efficiently as possible. STU is the standard measuring unit of autoclaving, measured in 30x30x60cm blocks.
Autoclave doors and control panels can be built in the most space efficient way possible. For example, though the control panel usually appears on the side of a large autoclave, it can be designed to be on top to make the machine narrower and thus a better fit for a tight space.
Large Autoclave Door Options
Another way to customize large autoclaves is with one of these four styles of one or two doors:
- R Door: Regular manual hinged door
- A Door: Automatic hinged door
- V Door: Vertical sliding door
- H Door: Horizontal sliding door

Pass-Through Autoclaves
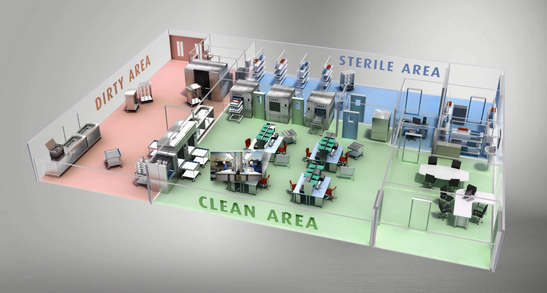
Many sterile processing departments have three distinct areas: dirty, clean, and sterile. Used surgical equipment comes straight from the operating room covered in bodily fluids and must be cleaned. This occurs in the “dirty” section of the department. After the equipment is thoroughly cleaned of all visible dirt, bodily fluids, etc., it is then disinfected in washer disinfector machines, which are located between the “dirty” and “clean” sections. Finally, once disinfection is complete, the equipment is ready for sterilization in an autoclave, which takes place between the “clean” and “sterile” areas, divided by a single or double wall separation. Disinfected equipment enters from a door facing the clean area and exits from a different door facing the sterile area. Also known as a pass-through autoclave, this system of two separate doors on each side of the autoclave allows for sterilized equipment to remain sterilized and not become recontaminated in the “clean” section of the department. By emerging in the “sterile” section, the autoclaved equipment is ready to be brought back to the OR or stored for future surgery.
Installations
How are large autoclaves installed? There are generally two methods.
The most common method is floor-standing autoclave installation. These autoclaves stand on the floor of the facility. Typically, the bottom of the chamber is about 90 cm above the floor.
The other type of installation is pit-mounted. A pit-mounted autoclave is installed in a pit in the floor so that the floor of the chamber aligns with the floor of the facility. This is advantageous for big and/or heavy loads, which can be loaded and removed easily by rolling the cart into the autoclave chamber. This type of installation is available for bulk large autoclaves, which are up to 18,000 liters.
The Rundown on the Large Autoclave
With its substantial capacity, the large autoclave is designed to process loads reliably and efficiently. In this way, large autoclaves are able to keep up with the high-volume demands of hospitals, and other medical/scientific settings.
Let’s review: we explored each step in the sterilization cycle:
- Air removal by negative pulses
- Pressurization of the chamber by positive pulses
- Sterilization time
- Release of pressure
- Drying stage
- Break of vacuum and end of cycle
We then investigated the autoclave jacket and why it is necessary to prevent cold spots inside the chamber. We also looked at how large autoclaves can be custom-built to fit narrow spaces. By providing different options in the layout of the sterilizer, for example with doors and control panels, sterile processing departments are able to make the most of their cramped quarters.
And that’s the rundown on the large autoclave. Come along with us on our next post about laboratory autoclave applications.
Comments and questions are welcome, as always, in the comment section below.