The previous “High Temp Sterilization Method Series” discussed the most common heat sterilization methods for loads not sensitive to heat and focused on the industry's favorite method (and of course our expertise) steam sterilization and steam quality. Now we'll explore low temperature sterilization methods for heat sensitive and moisture sensitive loads, with a series of posts opening the discussion with chemical and gas methods.
Why use alternative methods to steam? We have been praising sterilization by steam and we showed how it's ideal for destroying bacteria, fungi and spores. We mentioned it as being the most cost effective and simple method available, but steam is not applicable to all materials and instruments. Advancement in medical procedures has resulted in the increased usage of delicate instruments which cannot be steam sterilized. This is because they cannot withstand the higher temperatures or moisture of steam. Heat and moisture sensitive equipment require alternative methods of sterilization.
EtO gas is carcinogenic, explosive and mutagenic.
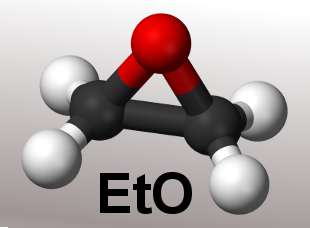
Let us open the discussion with a warning. The use of poisonous gasses should remain limited to sterilizing products for which no alternative methods are available. The obvious reason is that whatever kills microorganisms is lethal to humans as well. Most sterilization chemicals and gases are already endangering human health and even lives in very low concentrations. We should always consider that we need to do an in-depth risk analysis to see if using a poisonous gas is unavoidable. Ethylene Oxide (EtO) is a common gas used for low temperature sterilization. It is a colorless, poisonous gas that attacks the cellular proteins and nucleic acids of microorganisms. It is most commonly used to sterilize instruments with long lumens such as endoscopes and all materials that have to be sterilized but cannot withstand higher temperature. EtO process temperatures from 25 - 55°C are used. A lower temperature results in a less efficient process which leads to a longer exposure time.
EtO Sterilization Cycle
There are at least three stages in a typical EtO sterilization cycle:
- Preconditioning
- Sterilization
- Aeration (Degassing)
Cycle time is usually more than 14 hours.
Preconditioning
Preconditioning prepares the chamber environment to meet the ideal conditions for temperature, pressure and humidity. First air is removed from the chamber to allow for gas penetration. A leakage test is performed, to ensure that staff and environment are safe. Next, some steam is injected into the chamber and humidifies the load, since EtO is only effective in a humid environment. The chamber is heated by either steam or hot water which is present in the jacket. Normally the jacket is kept at the same temperature 24/7 to minimize temperature fluctuations.
Sterilization
The second stage is the actual sterilization process. The EtO enters the chamber via evaporation with a certain amount of steam to keep the humidity level up as well as to make sure the EtO is reaching all parts of the load. When the required concentration in the chamber and load is achieved the actual sterilization stage starts. The lower the gas concentration in the chamber the longer is the sterilization time. As EtO is absorbed by many kinds of plastic materials it is important to keep the concentration at the right level. To achieve this EtO is sometimes added to the chamber after a while. It is of major importance to ensure the appropriate concentration level of EtO in the chamber to achieve effective and safe sterilization.
Aeration (Degassing)
Aeration is the most important and longest part of the EtO sterilization cycle. As mentioned, materials such as plastics and rubbers absorb gas and if applied to patients, the toxic gas could damage their body tissue! For this reason it is very important to have an excessive aeration stage to remove any remaining EtO gas and to allow absorbed gas to evaporate again from the sterilized items. This is done by circulating HEPA filtered air over the load at a temperature of 30°C to 50°C. A commonly used time period for this aeration treatment is 48 hours which results in a very slow instrument turnaround. A special infrastructure is required, with gas tight ventilation piping to the roof top or to a catalyzer. The sterilizer cannot use the hospital's ventilation system because it is too dangerous. The special ventilation piping has to be tested for gas leaks all the way as this is the only way to minimize the risks.
There are some advantages, however. An EtO sterilizer can have a very large chamber, even up to 7m³. They are often used for the sterilization of large quantities of products that cannot be sterilized by steam. When gauze or non-woven materials like disposable gowning are manufactured, they need to be sterilized before entering the hospital. These are often sterilized by EtO because steam will damage or deform these materials.
To summarize, EtO sterilization should be used only when another method is not appropriate.
Advantages of EtO are:
- Low temperature
- High efficiency – destroys microorganisms including resistant spores
- Large sterilizing volume/ chamber capacity
- Noncorrosive to plastic, metal and rubber materials
Disadvantages are:
- Excessively Long cycle
- Safety concerns - carcinogenic to humans
- Toxicity issues - toxic residues on surgical instruments and tubing
- Not recommended for flexible scope
- EtO is flammable
- Requires special room conditions, safety equipment and separate ventilation system
- Relatively high annual costs for maintenance, servicing and consumables
