Haga click aquí para leer este texto en español
For both patients and hospital staff alike, germs must be destroyed in order to prevent the spread of infections. An important example of this is the fight against health-care-associated infections (HAIs), infections that hospital patients get as a result of their stay in the hospital. This may be due to contaminated equipment, surgical instruments, or improper staff hygiene.
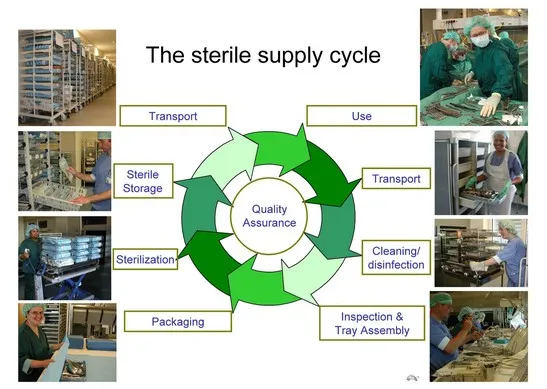
Every hospital must have a battle plan to prevent the spread of HAIs. The hospital’s germ warfare strategy consists of three processes, done in the following order: cleaning, disinfection, and finally, sterilization. Let’s take a look at these one by one, going from the weakest form of killing germs (cleaning) to the most severe (sterilization).
First Strike: Cleaning
When we use the term “cleaning,” we mean the removal of all visible dirt, dust or other foreign materials. This means that equipment that has been cleaned by hand with soap/detergent and water is free of all physical and chemical residues and is free of most microorganisms.
The goal of cleaning is to reduce the bioburden. The bioburden (or initial contamination) refers to the population of viable organisms on a material, instrument, product or package. Depending on where and how the item will be used, cleaning may be enough to reduce the bioburden, but for most other types of medical equipment, cleaning is only the first step, which will be followed either by disinfection alone or disinfection and then sterilization. In other words, cleaning is always the first step in the subsequent disinfection and sterilization of equipment.
There are five main reasons why cleaning all medical equipment is so crucial:
- It gets rid of all blood, pus, dirt or foreign particles that are left, which may cause dangerous complications for the next person to be operated on using that instrument.
- It reduces the bioburden.
- It takes away the breeding ground of surviving germs.
- It prevents the corrosion of highly precise and expensive tools, which have delicate hinges and pivots.
- It ensures the safe transfer of equipment to be assembled and packed for disinfection or sterilization.

Second Strike: Disinfection
When we use the term disinfection we mean the destruction of all vegetative (living) microorganisms, without necessarily killing all bacterial spores, a difficult-to-kill form of bacteria which exists in a kind of hibernation state that can withstand tough conditions.1 Some types of bacterial spores are very dangerous, e.g., anthrax, and tetanus. In order to kill ALL microorganisms, including bacterial spores, we must sterilize (see next section).
Hospital rooms may be disinfected with chemicals whereas medical equipment is placed inside an automatic washer machine (think dishwasher for tools instead of dishes). Items that come in contact with bodily fluids or feces, such as bedpans and urinals, need to be disinfected in a “washer disinfector” machine. But the vast majority of medical equipment will require disinfection and then sterilization.
A word about the terms disinfection and decontamination: In much of the medical industry, the terms decontamination and disinfection are used interchangeably. The problem with using the term disinfection when referring to medical equipment is that medical equipment can’t actually become infected in the first place; only people (or animals) can! Have you ever heard of a coughing needle or a feverish pair of scissors? No! Alas, while this term is not strictly correct, it is the one used most often to describe this second stage of the process. And as if that weren’t confusing enough, sometimes decontamination is used as a synonym for disinfection, but sometimes it refers to the whole “decontamination process,” which is another way of saying all three stages of cleaning, disinfection, and sterilization.

Final Strike: Sterilization
After our equipment has gone through the processes of cleaning and disinfection, it is ready for the last and most serious process of germ eradication, sterilization: the killing of all microorganisms, including bacterial spores. The World Health Organization recommends that all instruments that could possibly come in contact with fluids inside the body should be sterilized before use (ibid.).
The oldest method of sterilization is open-flaming, in which the item was held over an open flame to kill all germs (think: cavemen and an animal on a spit over an open fire.) In modern times, thankfully, there are more advanced methods of sterilization such as:
- moist heat
- dry heat
- biocide by gas or chemicals
- radiation
By far, the industry standard for sterilization today is to use pressurized high-temperature steam to kill all microorganisms in a specialized machine called an autoclave. Based on the model of the pressure-cooker, modern autoclaves run various cycles for different types of equipment and materials, as well as liquids. They come in different sizes, from small tabletop microwave oven-sized machines to large hospital elevator-sized machines. Depending on the needs of the hospital, there may be one or several autoclaves used on a daily basis to sterilize all equipment used during operations.
Battlefield: The CSSD
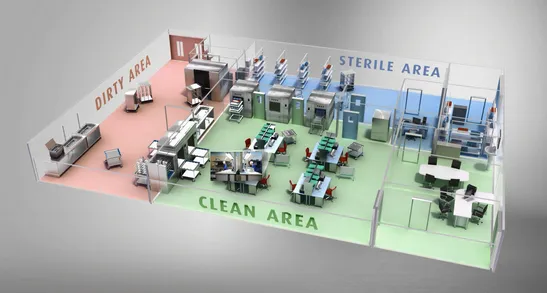
In every hospital there is a special department called the Central Sterile Services Department (CSSD) (or sterile processing department/SPD) where all cleaning, disinfection, and sterilization takes place. Each hospital’s CSSD works hard to ensure that once equipment and materials emerge from the autoclave that they stay sterile until opened in the operating room. There are specific protocols for how instruments must be packaged and handled before and after autoclaving to ensure that the items remain sterile and therefore don’t become recontaminated.
A Never-Ending Battle...
Unbeknownst to most hospital patients, the CSSD is where the never-ending battle against the spread of infection takes place on a daily basis. Suited up in their battle gear of scrubs, disposable gloves, caps, and masks, the technicians begin with their first line of defense, cleaning, which kills most of the disease-causing microorganisms with simple soap and water. Then comes the second line of defense, known as disinfection, which kills all vegetative microorganisms. And finally we go to the last defense, the take-no-prisoners strike of sterilization. There, in the autoclave, every last bit of microorganism, including the stubborn bacterial spore, is annihilated. The CSSD technician carefully stores the package of freshly sterilized tools until they are needed for the next life-saving operation in the hospital. Mission accomplished.
Check out our next post, “What is an Autoclave?” in which we will delve deeper into the concepts of autoclaving, finding out how and why they work.
Comments and questions are welcome, as always, in the comment section below.
(Post based on Sterilization of Medical Supplies by Steam by Jan Huys. Except for image of CSSD, all images appear with permission from Huys.)
1 Huys, Jan. Sterilization of Medical Supplies by Steam. mhp Verlag GmbH and Heart Consultancy, Wageningen, The Netherlands, 2010.