Although this survey shows that spring cleaning is in decline, many people still break out the mop and broom at this time of year and hum the spring cleaning song.
In the spirit of spring this post makes some order between the terms cleaning, disinfecting and sterilizing that are often confused. Spring cleaning is a great opportunity to bring the subject of infection control closer to our everyday lives.
Let's start with a short quiz: Which area in the house has the most bacteria?
- Kitchen Sink
- Toilet Seat
- Dish Sponge/Rag
- The trash can
Hope you'll stick with reading this post long enough to find out where you will find the right answer to the quiz.
It's All a Question of Bio-burden
Let's begin with understanding bio-burden.
Definition: Bio-burden is defined as the number of living organisms residing on a surface that has not been sterilized.
Now our quiz question can be rephrased as:
Which area in the house has the highest level of bio-burden?
In a hospital setting the level of bio-burden needs to be reduced to an acceptable level in order to eliminate or minimize the risk of infection. The preventative measures taken depend on where and how the instruments will be used. Sick people carry a wide variety and great number of bacteria, often infectious, therefore the area around them also needs to be maintained at acceptable bio-burden levels.
The measures taken to reduce bio-burden depend on the risk level. The highest risk levels occur with exposure to open wounds and penetrated skin or mucous membranes. Inner fluids of the body are an optimal breeding place for pathogenic microorganisms, germs, bacteria, viruses or spores, with ideal temperature and humidity conditions. Therefore there is zero tolerance for the existence of bacteria in all instruments and materials that will come into contact with an open wound or penetrate the body. Sterilization is a must for facilities where high level risk areas exist . Our previous posts discussed the different sterilization methods available, incineration being the most destructive of them all.

Incineration will ensure high sterility assurance levels (SLAs) but we don't recommend this tip.
At home sterilization is usually not required. After all it's not a common practice to perform surgeries in your home, but it is used to some extent. We sterilize a needle by burning it when we need to remove a thorn from the skin. We “sterilize” baby bottles and jars, even though we perhaps don't meet the standards and requirements of hospital sterilization levels, but in most cases the process done at home is safe and will destroy most of the germs.
Decontamination for Medium to Low Risk Areas
Medium risk areas are the mucous membranes. Decontamination is the process for killing the microorganisms on equipment for use in medium risk areas. Instruments in contact with medium risk areas, such as flexible endoscopes need high-level decontamination before each use. The most common methods of decontamination is by wet or dry heat or chemicals. Tuttnauer's line of washer-disinfectors decontaminate. (Side note: Today many countries have become stricter and are requiring sterilization for endoscopes. These stricter requirements have made low temperature sterilization more important as seen with the big demand for plasma low temp sterilizers that use vaporized hydrogen peroxide.)
Skin is considered a low risk area, and is a good protection against common microorganisms. However there are disease causing microorganisms that are able to be transferred via the skin. Therefore all active living microorganisms, which may be on instruments and materials that may be in touch with the skin have to be killed. Sterilization is required for these instruments and materials.
To summarize, disinfection is the process of eliminating or reducing harmful microorganisms from inanimate objects and surfaces whereas sterilization is the process of killing all microorganisms. Disinfection and sterilization are both decontamination processes.
Decontamination practices, also known as disinfection, are already more prevalent in the house than sterilization. Our dishwasher and washing machine, for example, use a cleaning detergent containing bleach to perform a simple form of decontamination.
Cleaning Almost Does it All
Finally we reach the most basic step, cleaning, which moves us from the invisible to the visible realm. This is what all of us do at home. By cleaning, which by definition is the removal of all visible dirt, dust or foreign materials, a major part of the microorganisms will be removed along with the dirt. In a clean house the body's immune system is usually enough to keep itself healthy. At home we use a broom, duster, cloth or vacuum cleaner. More thorough cleaning requires water, soap and a mop. After cleaning some microorganisms are left over, but their ability to multiply is reduced to a minimum because the moisture and nutrients have been removed. In hospitals the amount of germs is significantly larger and the patients are often weak and cannot fight them, therefore cleaning in a hospital is crucial, especially cleaning the area around and near the patient. Therefore cleaning is a safety practice. A clean house is a safe house and a hospital with sound cleaning habits is much safer.
Don't Undermine Cleaning
Medical supplies that are used directly on or in patients have to either be decontaminated or sterilized. But they first have to be cleaned; this step is mandatory. The visible dirt must be removed for several reasons: Even sterile dirt can cause damage if it enters a patient, because the body tends to reject any foreign matter. Cleaning already reduces the bioburden level therefore making the sterilization or the decontamination process more effective. Any dirt remaining on instruments can potentially cause corrosion, which is also dangerous for the patient.
Concluding Cleaning
We hope that now you gained some understanding when we use cleaning, decontamination and sterilization and why each stage is necessary.
Now back to our quiz. We asked you which area of the house has the highest level of bio-burden. The intuitive answer is the toilet seat (the average toilet bowl has 3.2 million bacteria per square inch, according the Centers for Disease Control and Prevention), but according to health expert Dr. Joseph Mercola, there could be up to 200 times more fecal bacteria on your kitchen cutting board than on your toilet seat. But without any doubt, the worst offender is the kitchen sponge, which can contain up to 50 million bacteria! Hands down, the kitchen sponge is where the germs live and thrive. Thoroughly wiping the sink and counters with a sponge serves only to spread them all over the kitchen, so beware to decontaminate your sponge periodically. There is no reason for alarm: most of the germs are fairly benign, and the body’s immune system is usually fit for fighting them off.
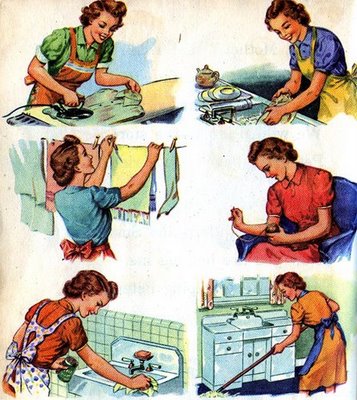
Spring Cleaning Removes Visible and Invisible Creatures
With all this knowledge we are confident you are on your way to making your house spic-and-span but for now, we'll let go of our fixation for a sterile home, unless you want one of these in your kitchen?

Happy Spring Cleaning from Tuttnauer