With Internet technologies, we can map and track the spread of diseases around the world in real time and with relative ease. It’s fascinating to follow how diseases spread, and sometimes it can be quite scary. MERS is grabbing global media attention as the latest disease on the rise. Much remains unknown about how MERS is transmitted, and a vaccine has yet to be discovered. We would like to introduce you to this mysterious visitor from the Middle East and show you how hospitals and health-care facilities work to prevent its spread.
The Latest Addition to the Corona Family - MERS
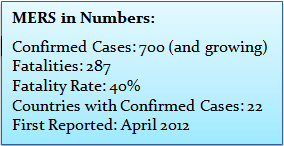
MERS-CoV, Middle East Respiratory Syndrome Coronavirus, is the virus that causes MERS. You’re probably familiar with Corona beer, but Corona is also a family of viruses, ranging from the common cold to SARS, which spread throughout China in 2003. Coronaviruses were first identified in the 1960s, but we don’t know where they come from. They get their name from their crown like shape. Discovered in 2012, MERS is the youngest member of the notorious coronavirus family. Research shows that MERS has long infected animals but only recently crossed over to humans.
Camels and Bats to Human Transmission
Researchers are still trying to track the origins of MERS. There is evidence that camels in Saudi Arabia were infected as far back as 1992. Before that, MERS attacked Egyptian tomb bats. These bats are found is South Africa and Asia but seem to transmit to people only in the Middle East.
The Virus seems to be adapting to humans, contributing to its spread.
Human-to-Human Transmission
MERS appears to spread among those in close contact, such as family members, patients, and health‐care workers. In some communities, people have become ill but no source of infection has been found.
MERS, Sterilization and Infection Control
What happens when MERS enters the health-care environment? There is quite a bit of spread within hospital settings. Most of the spike in cases this spring is due to hospital outbreaks in the UAE and Saudi Arabia. Hospitals are a great place for viruses to spread, since sick people are highly vulnerable to infection.
There have been clusters of cases in health‐care facilities, where human‐to‐human transmission appears to be very efficient, especially when infection prevention and control practices are inadequate. Nineteen kidney-failure patients contracted MERS in Jeddah, Saudi Arabia, probably due to poor decontamination procedures. It is very important to develop proper guidelines for infection prevention and preparedness in order to protect health-care providers and patients.
The good news: Proper infection control and sterilization procedures can easily beat MERS. Coronaviruses are fairly fragile. Outside the body, they can’t survive past a day and readily succumb to common cleaning agents. Standard disinfection and sterilization processes are adequate for sterilizing instruments or materials that have been contaminated by blood or other fluids of people infected with MERS. It is also important to decontaminate all wastes – often by steam sterilization – before disposal.
The Future of MERS
Millions of people around the world are expected to make the annual pilgrimage to Mecca, Saudi Arabia, during July 2014. Proper sterilization and infection-control procedures plus simple hygiene can prevent a pandemic. Let’s all keep our eyes open and hope the worst of MERS is behind us.
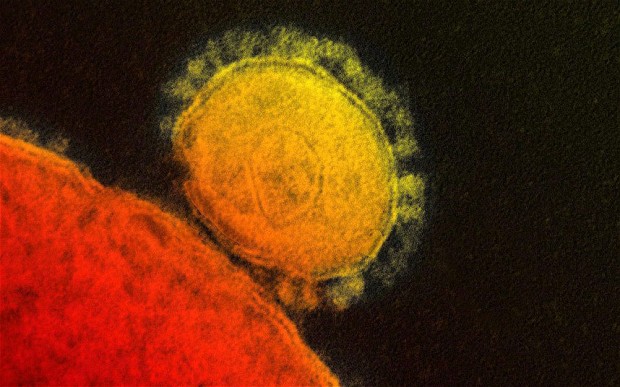
A close-up of the MERS coronavirus