Why does this matter?
The proliferation of superbugs means we are quickly running out of solutions to treat and save the lives of millions of people from seemingly benign bacterial infections like strep throat and ear infections. Instead we are facing new strains of old foes that are resistant to most or all kinds of antibiotics, and we don’t have the tools to fight them.
Two Temperature Sensors
In this post we’ll take a look at the real story behind superbugs:
- What are superbugs and why can’t antibiotics help?
- What do superbugs have to do with Hospital Acquired Infections (HAIs)?
- How can we prevent the spread of superbugs in hospitals?
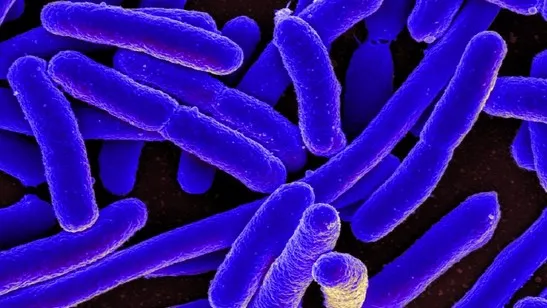
1. What are Superbugs and Why Can’t Antibiotics Help?
First, some background. Before the invention of penicillin in 1928 by Scottish scientist Alexander Fleming, there was no effective way to treat infections. In short, people either got lucky and healed, or they died. A scratch on someone’s skin that got infected could be enough to spell disaster. And then, with the new science of antibiotics, doctors were finally armed with a powerful weapon against bacterial infections. Over the last several decades, around a hundred different antibiotics have been developed and used to fight bacterial infections.
But there’s a catch.
Even Alexander Fleming admitted the potential danger of improperly using antibiotics. If too little penicillin was used or for too short a period of time, then antibiotic resistance would develop, thus allowing the surviving, strongest bacteria to make a comeback.
And this is what’s happening today: Often as soon as patients start feeling better, they stop taking the antibiotic before the course of treatment is completed. And that only kills off the weakest bacteria, leaving the strongest ones to survive and reproduce. In addition, “up to half of antibiotics used in humans are unnecessary and inappropriate.” There are common misconceptions out there about what antibiotics can do; for example, about a third of people believe that antibiotics can fight the common cold though antibiotics are actually useless against a cold. That’s because colds are usually caused by viruses, not bacteria! But treating the common cold is the most common reason antibiotics are prescribed!
And that’s just with humans. In the livestock industry, antibiotics are massively overused to keep animals healthy and fat in poor conditions, including tight quarters. About 80% of global antibiotic use is in factory farms. That is an astounding statistic. The overuse of antibiotics in animals gets passed through the ecosystem in our water supply, manure, and consumption of said animals, thus building up channels for superbugs to proliferate and grow stronger.
Some of the most well-known superbugs to hit the headlines in the last few years are:
- MRSA Methicillin-resistant Staphylococcus aureus
- C. difficile Clostridium difficile
- CRE Carbapenem-resistant enterobacteriaceae
- MDR-TB Multi-drug-resistant tuberculosis
- Antibiotic-resistant Gonorrhea
Here’s the deal. Superbugs are here to stay. The epidemic is no longer forecasted, but is now claiming lives all over the world; however, it is difficult to find data on global superbug impact since there are so many different bacterial diseases and regions of the world where they are spreading. According to the World Health Organization, “Antibiotic resistance is present in every country,” and “All countries need national action plans on AMR [anti-microbial resistance].”
In the United States alone, each year nearly two million people become infected with antibiotic resistant bacteria (which are resistant to at least one antibiotic), and 23,000 of those people die. Recently a woman in Nevada died from the CRE superbug, which is resistant to 26 different kinds of antibiotics. The Centers for Disease Control (CDC) director Dr. Tom Frieden has called CREs a “nightmare bacteria” due to the imminent danger they pose for spreading antibiotic resistance.
And the problem is compounded by the lack of new antibiotics being developed. “Following an unprecedented number of antibiotic discoveries in the last 40 years, the number of new antibiotics being identified has slumped to an all time low.” Pharmaceutical companies have, by and large, shifted their focus to more profitable endeavors like drugs that lower cholesterol and high blood pressure, and treat chronic diseases -- all medicines that are used on a daily, long-term basis. Investing millions of dollars into developing new antibiotics pales in comparison to the payoff of more lucrative drug sales, and there is a lack of funding and resources in the public sector to fully support this research.
2. What do superbugs have to do with Hospital Acquired Infections (HAIs)?
Now that we understand what superbugs are and how antibiotic use is making them grow faster and stronger, it’s time to take a look at the practical implications of how they spread. Most superbugs today are spread in hospital settings and are categorized as HAIs, or Hospital-Acquired Infections (also known as Healthcare-Associated Infections).
What is a HAI? It is an infection that the patient acquires during his hospital stay. There are lots of ways to contract HAIs, for example:
- Infected health care staff or other infected patients
- Improper staff hygiene
- Contaminated (surgical) equipment, air droplets, bed linens, and curtains
- Contamination by a microorganism found on the patient’s skin that enters a surgical wound site and successfully infects the patient in a high-risk, susceptible area
In the United States alone, the CDC estimates that there are about 1.7 million HAIs every year, which cause or contribute to 99,000 annual deaths. Estimates of the annual cost of treating HAIs in the US range from $4.5-11 billion (ibid.).
What’s the real story? Imagine the following: you go to the hospital for a fairly common hip replacement surgery. The surgery is a success, but you must stay in the hospital for several days to recover. On your second day of post-operative convalescence, instead of starting to feel stronger, you get weaker, have a high temperature and start showing signs of infection. You may have been infected by is a hospital-acquired infection (HAI). You go to the hospital for surgery or some other procedure, and end up sicker with a secondary infection.
But wait. What if the infection you contracted is a superbug? That means it is resistant to at least one, if not several kinds of antibiotics. Common HAIs occur in the urinary tract, the bloodstream, and surgical site; another common HAI is pneumonia. And if the one you contracted is a superbug, i.e., that it is resistant to at least one if not more antibiotics, well that’s going to make your recovery all the more difficult and expensive.
3. How Can We Prevent the Spread of Superbugs in Hospitals?
Besides practicing proper hygiene in hospital settings, one of the most important ways we can prevent the spread of superbugs in hospitals is to make sure all medical equipment is free of superbug contamination, i.e., properly sterilized. As a leading member of the sterilization and infection control effort, we at Tuttnauer understand the challenges involved. But failing to achieve sterilization means the likely spread of dangerous microorganisms from one patient to another via contaminated surgical instruments and other medical supplies.
This infographic from the CDC depicts how to prevent the spread of antibiotic-resistant HAIs and common forms of HAIs:

Donna Swenson’s important post on reprocessing medical devices underscores the obstacles to medical device reprocessing, including manufacturers’ instructions for use (IFU) for these devices, which are often easily misunderstood. In addition, many hospitals continue to use older devices despite documented problems of proper cleaning, disinfection, and sterilization. And moreover, many IFU’s don’t take into account how difficult it is to disassemble and reassemble delicate tools while wearing protective gloves. As she points out in the post, a device that is not properly cleaned initially will not be sterile when it emerges from the autoclave:
If a device is not clean then sterilizing it will not necessarily result in a sterile device. If during the cleaning process the microbial contamination on the device is not reduced to a level low enough for the sterilization process to work, then the device will not be sterilized. Both disinfection and sterilization rely on adequate cleaning. Sterilization does not override inadequate cleaning.
And even when the IFU is followed, there have been many cases recently of said devices spreading dangerous infections. Swenson explains:
There was the case of a Texas hospital that had a series of infections caused by using a dirty instrument (an arthroscopic shaver). In this case one of the patients who got an infection had part of his shoulder bone and rotator cuff eaten away by the infection. Recently in 2014 and 2015 there have been several documented cases where duodenoscopes have been implicated in causing a HAI known as carbapenem-resistant Enterobacteriaceae (CRE). In all of these cases the manufacturer’s instructions were followed but the disinfection or sterilization process was not effective because following the instructions did not result in a clean instrument.
Reporting
And finally, one last point about preventing the spread of superbugs. In many parts of the world, hospitals are not required to report superbug-related deaths. Even in the United States, for example, the news agency Reuters conducted an investigation into the country’s failure to adequately report superbug deaths. According to the report, government agencies and state health departments do not require hospitals to report superbug cases, and often hospitals are eager to hide the problem by leaving the multi-drug resistant bacterium off of the victim’s death certificate.
Not reporting superbug deaths presents a serious obstacle to tracking the outbreaks properly and ideally, preventing future ones. How can experts understand the problem if they don’t actually have the data to show where and why the outbreaks are occurring? As a side point, proper reporting was crucial in slowing the spread of HIV/AIDS.
On a global scale, proper reporting is a must. A WHO report reveals “major gaps in tracking antibiotic resistance” in many of the world’s regions, including Africa, Europe, and the Eastern Mediterranean. The report further emphasized, “... that key tools to tackle antibiotic resistance–such as basic systems to track and monitor the problem–show gaps or do not exist in many countries. While some countries have taken important steps in addressing the problem, every country and individual needs to do more.”
The Scary Success of Superbugs
In September 2016, the United Nations convened the High Level Meeting on Antimicrobial Resistance, marking only the fourth time in UN history that a health issue has taken center stage. At this global forum, world leaders and health experts declared antibiotic resistance “the greatest and most urgent global risk.” And now you understand why.
Superbugs are multi-drug resistant bacteria that have “outsmarted” our most powerful line of defense, antibiotics. Though we have developed about a hundred different types of antibiotics, these bacteria have evolved to survive their powers and have become increasingly more prevalent and stronger through spontaneous mutation and DNA transfer. We have helped these superbugs to proliferate by improperly prescribing them (often to treat viruses though antibiotics are NOT antivirals), not taking them as directed, and overusing them in the livestock industry.
We spoke about some of the most common superbugs in the last few years, as well as the scale of superbug infections. It is estimated that around two million people in the United States become infected with superbugs each year, and about 23,000 of them die from these infections.
And many, if not most, of the superbug infections documented are Hospital-Acquired Infections (HAIs). HAIs are secondary infections contracted in the hospital environment, often during or after surgery or other medical procedures.
Finally, we spoke of preventing the spread of superbugs in hospitals, which primarily means focusing our attention on the challenge of properly reprocessing medical devices so that they are free from contamination. As Donna Swenson argues, there is no way to successfully sterilize medical equipment that is still dirty when it goes into the autoclave. And the more sophisticated and delicate the surgical equipment has become, i.e., duodenoscopes and arthroscopic shavers, the more difficult it is to ensure successful sterilization.
Our last point was about the importance of hospitals and government agencies reporting superbug outbreaks, and only with this data can public health officials start to get to the bottom of the complexities of this real threat to global health.
What do you think is the greatest cause of superbug proliferation? Is it our overuse of antibiotics? The lack of education about what superbugs are? The spread of HAIs, which will increasingly be antibiotic-resistant? The lack of accurate reporting where superbug outbreaks are occurring? Or perhaps there’s another dimension of the problem you’d like to share. We’d like to hear your thoughts in the comments below!